Payer Rates for Healthcare Providers
Camber is providing access to ABA-specific reimbursement rate analyses for one of 100+ payors of your choice, based on the states where you provide services.
What is payor rate data, who can access it, and why does it matter? Learn more about the recent regulation that makes this data available, and how these changing policies are impacting the ABA industry.
We're also looking for your feedback so we can improve this resource for the entire industry. See your own rates represented accurately? Please let us know!
Request the data here
In 2020, the Transparency in Coverage final rule released by the Department of Health and Human Services (HHS) required insurance payors to disclose price information to the public.
Before this ruling in October 2020 (CMS-9915-F), insurance payors were able to use antitrust laws to withhold the rates they paid individual providers from the public. This new ruling mandated that all health plans must share their contracted rates for all providers, starting in July 2022.
Unfortunately, this data remains inaccessible for most providers.
While the HHS ruling mandates that insurance payors disclose rate files publicly on their websites, the CMS itself also acknowledges that "specific technology may be needed to download and read these files given their size and complexity" (source).
For instance, UnitedHealthcare maintains ~42K files worth of data, many of which are too large to download onto most personal computers, much less analyze individually.
So while rates are technically available, they're not useful for the vast majority of providers that don't have dedicated technology teams and resources.
As an ABA-focused technology firm, we've been able to extract, analyze, and visualize insurance rate data for ABA providers.
Take the graph on the page, which visualizes in-network 97153 reimbursement rates for United Healthcare in New Jersey.
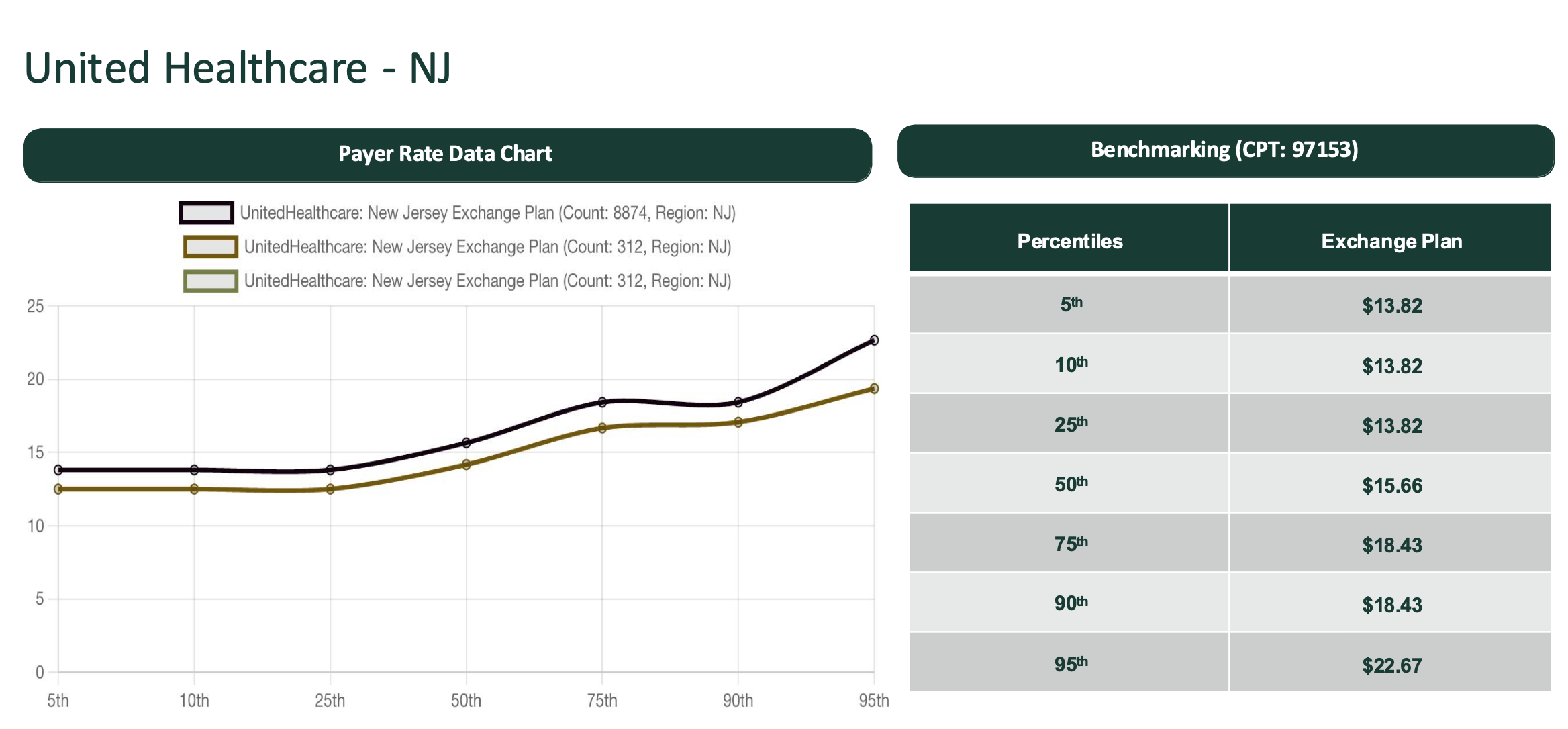
The X-axis gives the aggregated data percentile. The Y-axis reflects the reimbursement rate per 15-minute 97153 unit. For instance, a $13.82 unit in the 25th percentile means 25% of people make the same or less, while 75% make the same or more.
—
*We've compiled this data from insurance payor machine-readable files, the NPPES database, and other demographic datasets. While the names of individuals providers are included in the public dataset, we've aggregated the data by region for privacy reasons.
ABA providers can leverage this data to understand and strategize potential reimbursement rates specific to their insurance payors and service regions.
These insights can be an asset during the contracting and credentialing process.
Providers can also gain pricing information in neighboring geographies to help strategize how they might best serve certain regions sustainably.
But our data is only as accurate as insurance payors choose to disclose, and we're looking for your feedback to make it better. Do you know of rates that are not represented in the datasets as expected? Please let us know so that we can improve this resource for all of us in the community.
*Insurance payors each have their own contracting and credentialing process, for which there can be many factors that determine negotiated rates.
Request the data here
*Camber is continuously expanding its coverage of payors across different states. In the case that we don't have access to your specific payor region dataset today, your request will help inform where we prioritize our future coverage.
Camber does not participate in discussions or negotiations between providers and payers